Laryngotracheal cleft information
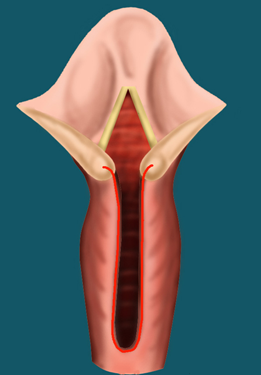
The development of the larynx (voice box) and its separation from the esophagus (food pipe) is a complex process. When the larynx develops normally, it is completely separate from the esophagus, so swallowed foods go directly into the stomach.
Laryngeal cleft is a rare congenital defect, though its occurrence has been under-reported in the medical literature. The dividing wall between the airway and food pipe is absent and communicates them directly, thus allowing passage of saliva, food and liquids into the lungs. These episodes of bronchoaspirations cause lung infections. The condition may be seen with certain syndromes (Opitz, Pallister-Hall, VACTERL, and CHARGE) and may be associated with other midline defects affecting the esophagus, heart, palate and vertebral column.
Signs and symptoms
Symptoms include:
- Feeding difficulties and false passage of food, liquids and saliva into the lungs (bronchoaspiration)
- Recurrent episodes of pneumonia ( lung infections)
- Chronic cough
- Stridor
- Symptoms related to floppy trachea and bronchi (refer to information on tracheo / bronchomalacia)
- Respiratory distress
- Symptoms due to associated midline anomalies.
Diagnosis
The diagnosis is made by performing a flexible and rigid endoscopy. The entire larynx, trachea and the esophagus are evaluated. Using a telescope, the back of the larynx is inspected and palpated with a microinstrument for a split between the larynx and esophagus. The next step is to determine the extent and length of this defect. The length of the defect decides the further management.
Depending on the cleft severity, following types have been proposed:
- Type 1: clefts are superficial and spare the cricoid cartilage.
- Type 2: clefts extend through the cricoid cartilage.
- Type 3: clefts splits upto the upper trachea.
- Type 4: clefts are the most severe with extension into the thoracic portion of the trachea and even into the bronchi. Such neonates have severe bronchoaspirations and poor lung condition and hence may not be compatible with life.
The esophagus is evaluated for acid reflux which is a common association with laryngeal clefts. A multi disciplinary approach is needed for children born with syndromes. They could have multi organ involvement and require a holistic approach in their management. These various special consultations are well established at the Lausanne University Hospital.
Treatment
The treatment depends on the severity of the laryngotracheal split, signs, symptoms as well as the other associated medical conditions. The child will have a tube passed into the lower digestive tract (jejunum) to allow nourishing the child and also reduce gastro-esophageal reflux and thus protect the lungs.
It is important to diagnose this condition early, especially in cases of chronic bronchopulmonary aspirations. Our experience has been that it is extremely under reported. We have had a case when the cleft had not been detected as late as 8 years, and the child was referred to us only with occasional episodes of aspirations. Incidently, this child was diagnosed to have a type 3 cleft and underwent a successful repair. Similarly, type 1 clefts may present late with very little complaints.
Most type 1, 2 and some Type 3 are repaired endoscopically. Type 4 clefts and when the cleft cannot be exposed well during endoscopy require an open surgical repair.
Our center is credited for performing the first ever endoscopic closure of a laryngeal cleft using laser and without the need of passing a tube in the airway and tracheostomy (Sandu et al, Laryngoscope 2006). Ever-since, we now have a large experience in treating this condition. World over, the endoscopic repair has become the standard method of treatment for laryngeal clefts.
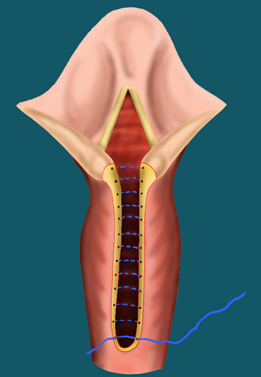
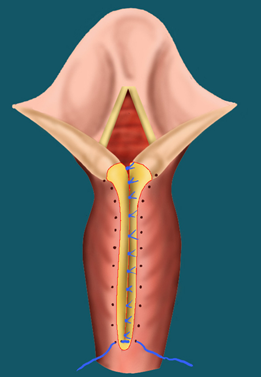
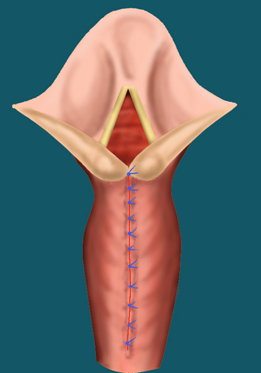
Endoscopic Treatment
In this procedure, the CO2 laser is used to freshen the edges of the cleft. Resorbable sutures are then used to close the cleft.
The child is given antibiotics to prevent infections and treatment for acid reflux.
Treatment for severe cases
Longer clefts are corrected by an external approach through the neck and chest. Clefts that extend low down in the chest are operated by a team of ORL and cardiac surgeons. Sometimes a very long cleft may extend into the bronchi and needs an appropriate correction.
Largely, the treatment of laryngeal clefts depends on the severity of the cleft and associated comobidites.
Complications
The main risk involved in the endoscopic or the open approach is a residual fistula between the trachea and esophagus. This needs to be closed by a second operation with an incision in the neck.
Follow-up care
Patients who have undergone an endoscopic repair start feeds on the next day or couple of days after surgery. Check endoscopy is performed at 7-10 days. Once the child has been well assessed to take adequate oral feeds he can prepare going back to his parent country (about 2-3 weeks). A final check endoscopy is done depending on the clinical symptoms of the patient.
For patients staying outside Switzerland, a systematic plan of follow up is prepared taking into consideration the long distance of travel and individual country insurance policies.



